5 Minute HealthTech Jargon Buster: Artificial Intelligence for Clinical Trials
- Romilly Life Sciences

- Jul 9, 2025
- 7 min read
By Lilian Hall, Research and Communications Associate
Clinical trials are research studies aimed at making medical advances and evaluating improved treatments [1]. The growing cost and complexity of clinical trials increases the workload of researchers and time to organise the trials, serving as a key area for development [2].
Clinical trials have extensive durations, requiring many phases. These include pre-clinical requirements such as: recruitment of relevant participants, gathering consent, scheduling a baseline visit. There are also requirements throughout and post-trial: continuous monitoring of participants, analysis of data, gaining regulatory approval and expanding the product to a larger population [1]. These components add to the duration and complexity of managing clinical trials.
Technology in Clinical Trials
The growth of technology and its use in clinical trials provides an abundance of opportunities to improve efficiency and management. Technology can be utilised in various areas including more efficient documentation, preclinical predictions, centralising data and improving consent.
Electronic health records
Documentation was previously on paper, however, electronic medical records are an electronic source of documentation, to help store and manage patient records on an online format [2]. Electronic health records (EHRs) offer numerous benefits for clinical trials, making research more efficient and cost-effective. They enable faster patient recruitment by identifying eligible participants through existing medical data. EHRs also streamline data collection, reducing manual entry errors and improving accuracy [3]. Additionally, they support real-world evidence studies by integrating research into routine clinical care, making findings more applicable to everyday practice. By automating processes, EHRs save time, lower costs, and enhance the overall quality of clinical trials [3].
Clinical trial management systems
Software platform developments such as the clinical trial management system (CTMS) offer multiple improvements to clinical trials. CTMS is a type of software platform which manages clinical trials, centralising the data collected from multiple sources. They are often used in conjunction with electronic health records to provide integrated data. Additionally, CTMS provides compliance support by maintaining accurate documentations, which can be used during audits and proof of FDA compliance.
eConsent
Patient consent is critical in participating in trials; thus, the prevalence of electronic consent (eConsent) provides an opportunity for consent to be monitored via an electronic system. This increases participant engagement through interactive features, such as videos and diagrams. EConsent has real-time tracking features, which allows for continuous monitoring and updating of consent throughout the trial. This ensures compliance and patient tracking [2].
Artificial Intelligence for Clinical Trials
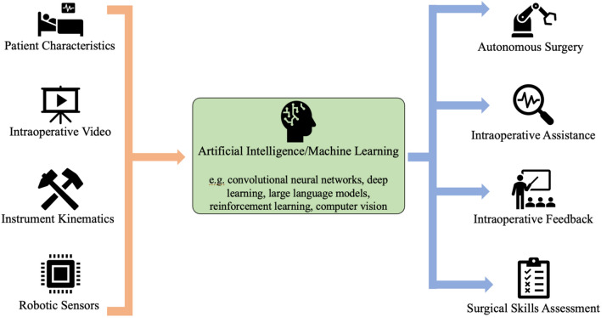
Artificial intelligence (AI) presents an opportunity to improve efficiency and time management of clinical trials throughout multiple stages. Figure 1 displays an overview of key opportunities, such as preclinical use and analysis and the challenges of AI in clinical trials.
![Figure 1. An overview of opportunities and challenges of using artificial intelligence in clinical trials. [4]](https://static.wixstatic.com/media/91ba22_d71359cd45cf4dfdb84b92d7f4ac20bc~mv2.png/v1/fill/w_902,h_672,al_c,q_90,enc_avif,quality_auto/91ba22_d71359cd45cf4dfdb84b92d7f4ac20bc~mv2.png)
Detection of drug toxicity
AI is significantly improving drug development, particularly in the preclinical stages, by enhancing both efficiency and safety. One of its most valuable applications is predicting drug toxicity, as highlighted in Figure 2, enabling researchers to identify high-risk compounds much earlier in the development process. By utilizing machine learning models trained on extensive datasets, AI can accurately assess potential toxicity, which helps reduce the need for traditional in vitro testing. This not only shortens the timeline for drug development but also lowers costs by filtering out unsuitable compounds before they advance to clinical trials.
Drug design and adverse effects
Furthermore, AI plays a critical role in identifying potential adverse effects early, helping to prevent harm to participants in clinical trials and reducing risks associated with post-market exposure. By providing these early insights, AI allows for better-informed clinical decision-making regarding the safety and design of drugs. This contributes to faster market access for drugs while minimizing financial losses that could arise from costly errors in drug development. As a result, AI’s integration into preclinical trials enhances the overall success rates and safety of clinical research. [5]
![Figure 2. The use of artificial intelligence in preventing drug toxicity in both preclinical and post market stages [5]](https://static.wixstatic.com/media/91ba22_bab92bb7bcab47c6afb4d6377e7233d0~mv2.png/v1/fill/w_642,h_732,al_c,q_90,enc_avif,quality_auto/91ba22_bab92bb7bcab47c6afb4d6377e7233d0~mv2.png)
An example of utilising AI in preclinical stages is in oncology trials. AI was used to streamline participant recruitment. Cloud-based AI systems can scan electronic health records and databases to identify eligible participants based on predefined inclusion and exclusion criteria. This approach enhances recruitment efficiency while reducing the workload on clinical staff, making the process faster and less labour-intensive [2].
Trial classification
Additionally, AI clinical management systems can be utilised to organise patient visits. For example, via the use of an automated trial classification system. This system categorises clinical trials, based on specific criteria, using algorithms and machine learning models to do so. For example, automated trial classification systems have been used to facilitate patient-trial matching to find individuals living with HIV and pregnant women. Using AI is particularly valuable as there were large datasets for recruitment, which would take clinicians a long time to manage [6].
Challenges when using AI in Clinical Trials
Whilst the use of AI proves advantageous in many areas, concerns remain regarding its use including the risk of bias, lack of transparency and privacy concerns. [7]
Biased data to train AI tools
One of the key limitations of using AI in clinical trials is the quality and representativeness of the data used to train these models. If the data used to train AI contains biases, those biases will be embedded in the model and carried through in its predictions. Essentially, if the dataset is not representative of the patient population or clinical scenarios, the AI-generated predictions could be inaccurate, which can have serious consequences. For example, if the data used to train the model overrepresents certain groups or underrepresents others, it could lead to skewed predictions of clinical outcomes. This could result in the overestimation or underestimation of risks to patients, which can directly impact their safety and the overall effectiveness of treatments [7]. Furthermore, the lack of robust and standardized datasets compounds this issue. Inconsistent or incomplete data can prevent AI models from being properly trained, limiting their ability to make accurate predictions. As a result, clinical trial outcomes might be influenced by data that doesn't fully reflect the real-world diversity and complexities of patient populations, creating significant challenges in the use of AI in clinical trials [4].
Unstandardised protocols between stakeholders
Another major challenge is the collaborative effort required to build and maintain comprehensive data repositories. AI in clinical trials requires input from various stakeholders, including researchers, clinicians, and regulatory bodies, to create the infrastructure necessary for its successful application. However, the fragmented nature of data collection practices and the lack of standardised protocols often make this effort more difficult [4].
Interpretability concerns
Interpretability of AI models also presents an issue. For AI tools to be trusted and widely adopted in clinical trials, particularly in complex fields like oncology or drug discovery, it's crucial to understand how the AI model reaches its predictions. The complexity of AI models, particularly machine learning (ML) algorithms, can make their predictions difficult to interpret. This becomes a significant concern, especially in the early phases of research, where understanding the biological mechanisms behind a model's output is essential [4].
Ethical considerations
Ethical concerns are one of the greatest issues with implementing AI. It is essential that the patient data used to train the model has been obtained with appropriate consent. Additionally, whilst data provided is typically anonymised, there is a risk that it could be re-identified, breaching patient confidentiality [7].
Regulations and Policy Considerations
Regulatory and policy concerns are crucial for implementing AI in clinical trials, focusing on data integrity, patient safety, and compliance with guidelines. Agencies like the FDA and EMA are working to ensure AI methods align with existing frameworks, prevent biases, and maintain ethical standards in clinical research.
FDA Strategies for the US
Regulatory and policy concerns surrounding the implementation of AI in clinical trials focus on ensuring data integrity, patient safety, and compliance with existing regulatory frameworks to offset the use of AI. According to the FDA [8] the use of AI in clinical trial design must align with established guidelines to prevent biases in data collection, ensure transparency in decision-making, and maintain ethical standards in patient recruitment and monitoring.
Additionally, the FDA highlight concern about the reliability and reproducibility of AI-driven models used in drug development, emphasizing the need for rigorous validation and regulatory oversight to ensure that AI-generated insights are scientifically robust and do not compromise patient outcomes [9]. As AI continues to evolve, regulatory agencies must establish clear policies that balance innovation with safety, ensuring that AI-driven methodologies enhance, rather than undermine, the integrity of clinical trials.
EU Strategies
The European Medicines Agency (EMA) has outlined its Regulatory Science Strategy to 2025, emphasizing the need for a robust regulatory framework for AI in clinical trials. Pharmaceutical sector stakeholders are working alongside academia and expert centers to develop guidelines for AI validation and assessment, ensuring the safe and effective integration of AI-driven technologies in clinical research [10].
Whether planning a clinical trial to evaluate new technology, including AI solutions, or developing new technologies that can enable improved clinical trial design and delivery, Romilly Life Sciences can offer several decades experience both utilising and pioneering new technologies in clinical trials.
To find out how you can reach patients faster, contact us.
References
[1] National Institute on Aging. “What Are Clinical Trials and Studies?” National Institute on Aging, 22 Mar. 2023, www.nia.nih.gov/health/clinical-trials-and-studies/what-are-clinical-trials-and-studies.
[2] Barlow, Candida. “Oncology Research: Clinical Trial Management Systems, Electronic Medical Record, and Artificial Intelligence.” Seminars in Oncology Nursing, vol. 36, no. 2, Apr. 2020, p. 151005, https://doi.org/10.1016/j.soncn.2020.151005. Accessed 3 Aug. 2021.
[3] Mc Cord, Kimberly A., and Lars G. Hemkens. “Using Electronic Health Records for Clinical Trials: Where Do We Stand and Where Can We Go?” Canadian Medical Association Journal, vol. 191, no. 5, 3 Feb. 2019, pp. E128–E133, https://doi.org/10.1503/cmaj.180841. Accessed 21 Nov. 2020.
[4] Askin, Scott, et al. “Artificial Intelligence Applied to Clinical Trials: Opportunities and Challenges.” Artificial Intelligence Applied to Clinical Trials: Opportunities and Challenges, vol. 13, no. 2, 28 Feb. 2023, link.springer.com/article/10.1007/s12553-023-00738-2, https://doi.org/10.1007/s12553-023-00738-2.
[5] Basile, Anna O., et al. “Artificial Intelligence for Drug Toxicity and Safety.” Trends in Pharmacological Sciences, vol. 40, no. 9, Sept. 2019, pp. 624–635, tatonettilab.org/archives/BasileYahiTatonetti-AI4DrugSafety-final.pdf, https://doi.org/10.1016/j.tips.2019.07.005.
[6] Zhang, Kevin, and Dina Demner-Fushman. “Automated Classification of Eligibility Criteria in Clinical Trials to Facilitate Patient-Trial Matching for Specific Patient Populations.” Journal of the American Medical Informatics Association, vol. 24, no. 4, 19 Feb. 2017, pp. 781–787, https://doi.org/10.1093/jamia/ocw176. Accessed 2 Sept. 2021.
[7] Reddy, Sandeep, et al. “A Governance Model for the Application of AI in Health Care.” Journal of the American Medical Informatics Association, vol. 27, no. 3, 4 Nov. 2020, pp. 491–497, academic.oup.com/jamia/advance-articleabstract/doi/10.1093/jamia/ocz192/5612169.
[8] “The Role of Artificial Intelligence in Clinical Trial Design and Research with Dr. ElZarrad.” FDA, 12 June 2024, www.fda.gov/drugs/news-events-human-drugs/role-artificial-intelligence-clinical-trial-design-and-research-dr-elzarrad. Accessed 2 Aug. 2024.
[9] FDA. “Artificial Intelligence for Drug Development.” U.S. Food and Drug Administration, 2024, www.fda.gov/about-fda/center-drug-evaluation-and-research-cder/artificial-intelligence-drug-development.
[10] European Medicines Agency. “Joint HMA/EMA Workshop on Artificial Intelligence in Medicines Regulation | European Medicines Agency (EMA).” European Medicines Agency (EMA), 28 May 2021, www.ema.europa.eu/en/events/joint-hma-ema-workshop-artificial-intelligence-medicines-regulation. Accessed 19 Mar. 2025.


Comments