5 Minute Healthtech Jargon Buster: Clinical Decision Support Systems
- Romilly Life Sciences

- Dec 19, 2023
- 6 min read
Clinical decision support (CDS) provides timely information, usually at the point of care, to help inform decisions about a patient's treatment. CDS tools and systems help clinical teams by taking over some routine tasks, warning of potential problems, or providing suggestions for the clinical team and patient to consider [1].
A clinical decision support system (CDSS) is a software application that analyses data to help healthcare providers make decisions and improve patient care.

Image Credit: Visensia® from Oxford Biosignals Ltd. is one of the earliest examples of an FDA-approved clinical decision support system that employs machine learning to predict which patients are at risk of deterioration, hours before most healthcare professionals can.
Objectives for a Clinical Decision Support System
A CDSS focuses on using knowledge management to generate clinical advice based on multiple sources of patient-related data. It offers information to clinicians and primary care providers to improve the quality of the care their patients receive. CDSS tools can, for example, offer reminders for preventive care, give alerts about potentially dangerous drug interactions and alert clinicians to possible redundant testing their patient has been scheduled to undergo. As such, using a CDSS can lower costs and increase efficiency [2].
As CDSSs become increasingly sophisticated in terms of the information they can generate, questions naturally arise about whether they are in fact diagnostics and when and how medical device regulations should be applied to them.
Examples of Clinical Decision Support Systems
CDSSs can include a wide variety of decision-making aids, such as computerized alerts and reminders to care providers and patients; clinical guidelines; condition-specific order sets; focused patient data reports and summaries; documentation templates; diagnostic support, and contextually relevant reference information, among other tools [3].
Clinical guidelines and diagnostic support frameworks do not have to be digital, but the modern definition of CDSS tends to focus on health IT applications, modules, or analytics that leverage an organization’s big data assets [4].
Clinical Decision Support Systems and the Role of Artifical Intelligence
Traditional CDSSs are considered knowledge-based and consist of three parts [5]:
The knowledge base contains the rules and associations of compiled data which most often take the form of IF-THEN rules. If this was a system for determining drug interactions, then a rule might be that IF drug X is taken AND drug Y is taken THEN alert the user. Using another interface, an advanced user could edit the knowledge base to keep it up to date with new drugs.
The inference engine combines the rules from the knowledge base with the patient's data.
The communication mechanism allows the system to show the results to the user as well as have input into the system.
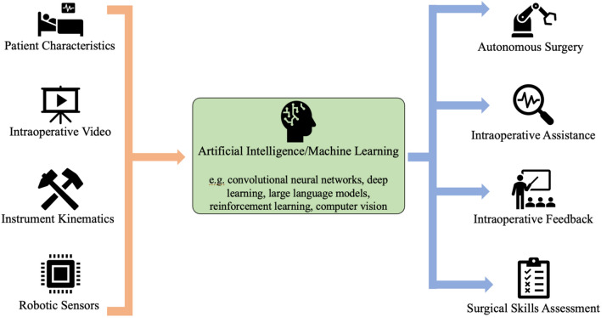
CDSSs which do not use a knowledge base use a form of artificial intelligence called machine learning, which allows computers to learn from past experiences and/or find patterns in clinical data. This eliminates the need for writing rules and expert input. However, this can make it harder for these systems to explain the reasons for their conclusions - needed for diagnoses, reliability, and accountability reasons - which motivates specific approaches to design and clinical evaluation which are described below.
Machine learning, which enables a range of different approaches, is well-suited to CDSS which seek to quickly and reliably identify patterns spread across multiple sources of clinical data while at the same time automating expert tasks such as patient examination and real-time monitoring.
Alert Fatigue
A core requirement of any data-driven solution for healthcare is that it simplifies the already-complex tasks of patient care by providing reliable, easy to interpret insights and does not instead simply generate more complex data that risks confusing the healthcare professional, even to the point of ignoring the system entirely. This is particularly true of CDSS whose role is to alert or warn users working in busy environments such as hospitals [6].
CDSS alerts can save lives, but frequent insignificant ones might cause alert fatigue. Studies discuss that 33% to 96% of clinical alerts are ignored. A CDSS has the p[otential to generate a high number of inappropriate alerts that interrupt the clinical workflow. As a result, clinicians will silence, disable, or ignore alerts, thereby undermining patient safety. This behaviour is known as alert fatigue. Many CDSS alerts were not properly designed based on human factor methods and principles, explaining high alert overrides in clinical practices [7].
Fortunately, we can learn from other safety-critical applications, including aviation and surgery, where alert-fatigue is well understood and mitigating strategies can be studied and applied [8].
Evidence-based strategies to reduce alert fatigue and improve CDSS utilization can be categorised into five major areas:
Classify alerts in to three main levels; severe, moderate and minor then develop a core set of critical drug to drug interactions.
Classify alerts into active and passive groups, where only critical alerts should be interruptive actively while less critical alerts should be non-interruptive to the user.
Conduct regular user training on new improvements.
Keep monitoring alert response rates and keep ongoing research and improvement efforts.
Provide systems with automated feedback and learning mechanisms where frequently ignored and justified alerts could be moved automatically from the active interruptive to the passive non-interruptive model.
When developing CDSSs, manufacturers should ask users during development, testing and implementation: “At what point does the alert hurt you?”
Regulation of Clinical Decision Support Systems
As the line between CDSS and diagnostic can be subtle if not blurred, recent guidance from authorities such as the FDA has provided clarity on the mandatory regulations for these tools [9]. Unless the CDSS meets all four of the following criteria, it will need to be regulated as a medical device.
Criterion 1: The software function is not intended to acquire, process, or analyse a medical image or a signal from an in vitro diagnostic device or a pattern or signal from a signal acquisition system
Criterion 2: The software function is intended for the purpose of displaying, analysing, or printing medical information about a patient or other medical information (such as peer-reviewed clinical studies and clinical practice guidelines)
Criterion 3: The software function is intended for the purpose of supporting or providing recommendations to a healthcare professional about prevention, diagnosis or treatment of a disease or condition and
Criterion 4: The software function is intended for the purpose of enabling such healthcare professional to independently review the basis for such recommendations that the software presents so that it is not the intent for such healthcare professional to rely primarily on any of such recommendations to make a clinical diagnosis or treatment decision regarding an individual patient.
How to Evaluate Clinical Decision Support Systems
Many examples of CDSS seek to predict an event ahead of time, for example a patient needing to be admitted to intensive care, so that it can be preventatively managed or averted entirely and as a result the concept of a “silent trial” has gained some popularity. This is where a CDSS is operated alongside existing clinical practise and the predictions offered by the CDSS are compared to what transpires in practise, not yet allowing for intervention based on the prediction itself.
This early clinical evaluation provides a crucial scoping evaluation of clinical utility, safety and human factors challenges in live clinical settings. By investigating the potential obstacles to clinical evaluation at scale and informing protocol design, these studies are also important stepping stones toward definitive comparative trials.
However, the strongest evidence for these tools is when they can be shown to measurably improve patient outcomes, for which a full clinical study is required [10]. Here there is a substantial body of guidance on risk management [11], reporting clinical benefit in a replicable manner including human factors such as alert fatigue [12] as well as more generally across diagnostic and prediction technologies to guard against the risk of bias [13].
Where to find out more
Romilly Life Sciences can offer several decades experience leading the validation, regulatory approval and implementation of clinical decision support systems as well as now-routinely deployed machine learning solutions for decision support in other safety-critical industries such as aviation.
To find out how you can reach patients faster, backed by compelling evidence, contact us.
References
[4] https://healthitanalytics.com/features/understanding-the-basics-of-clinical-decision-support-systems
[5] Berner, Eta S., ed. Clinical Decision Support Systems. New York, NY: Springer, 2007.


Comments