5 Minute Healthtech Jargon Buster: Telehealth
- Romilly Life Sciences

- Sep 30, 2024
- 9 min read
by Hannah Croft, Research and Communications Associate
In a world where technological innovation constantly reshapes our daily lives, telehealth stands as a beacon of progress in the realm of healthcare. The COVID-19 pandemic has highlighted the revolutionary potential of telehealth, transforming how we deliver and access healthcare. As technology professionals, the shift presents a unique opportunity to redefine patient care. The future of healthcare is here, driven by telehealth’s innovations – let’s explore how this evolution is shaping the industry and what it means for you.
Credit: Gregory Marcus, UCSF
Telehealth involves the use of information and communication technologies to deliver patient care and healthcare services remotely, “beyond the doctor-patient relationship”. It encompasses a wide range of activities including medical care, social support, and medication adherence [1].
Telemedicine is a subset of telehealth that specifically involves the provision of clinical services to patients through telecommunications technology. This includes remote clinical consultations, diagnosis, treatment, health monitoring and disease prevention by healthcare professionals [1].
Telecare specifically refers to technology-enabled personal care and support services for individuals, particularly the elderly or those with chronic conditions, allowing them to live independently and safely. It often includes devices and services that monitor daily activities and health status, providing alerts & responses to ensure the individual’s well-being [1].
Although the focus of this article is on the broader subject of telehealth, providing definitions for telemedicine and telecare highlights the more nuanced differences and interconnections within the field.
Benefits
Access to Healthcare
Improves access to healthcare facilities over distance and outside working hours from home or any location [2].
Reduces wait times and can provide quicker access to specialists
Extends healthcare to areas which are remote, rural or with limited resources or dense populations [3]
Cost & resource efficiency
Lowers healthcare costs by reducing travel expenses, hospital admissions, and in-person visit requirements [4]
Enhanced Quality of Care
Facilitates continuous monitoring and early intervention, improving health outcomes.
Encourages patient engagement and self-management of health conditions, as well as adherence to good lifestyle habits and treatments [4].
Improved Coordination and Efficiency
Streamlines administrative processes and enhances communication among healthcare providers.
Facilitates integrated care by ensuring that all providers have access to up-to-date patient information [5].
Enhanced Patient-professional interaction
Strengthens the patient-professional relationship by facilitating virtual communication.
Provides timely and relevant health information [3].
Key technologies
Teleconsultations facilitate virtual meetings between patients and healthcare professionals, as well as between primary care physicians and specialists. Patients can connect with their doctors remotely through secure messaging, video or phone calls; ensuring convenient access to medical advice, diagnosis and treatment. Simultaneously, physicians can consult specialists in real-time, sharing patient information, diagnostic images and expert opinions to provide coordinated and comprehensive care, all without the need for travel or secondary referrals [6].
Remote Patient Monitoring (RPM or RM) involves the use of digital devices to track and share patient health data, such as vital signs, from their home to healthcare providers. This continuous monitoring allows for early detection of potential health issues, timely interventions and personalised care management, improving patient outcomes and reducing the need for frequent in-person visits [6].
Mobile Health (mHealth) utilises smartphones, smartwatches, tablets and mobile apps to deliver healthcare services and information. These tools empower patients to manage their health through features like medication reminders, symptom trackers, sleep monitoring, and fitness tracking applications. Specific apps, such as Type I diabetes management apps, Anaemia monitor apps and Doctor meal plan apps, offer specialised support, enhancing patient engagement and accessibility to tailored health resources. The use of mHealth applications is also associated with increased patient satisfaction, as they provide convenient and personalised healthcare solutions [7].
Electronic Health Records (EHRs) are digital versions of patients’ medical histories, treatments and diagnoses that are stored securely and accessible to authorised healthcare providers. EHRs streamline healthcare delivery by enabling efficient data sharing among healthcare teams, improving accuracy in diagnoses and treatments, and enhancing patient safety through comprehensive health information management [8].
Online Portals are secure websites or applications that allow patients to access selected information from their EHRs, communicate with healthcare providers and manage their care. These portals enable patients to view lab results, schedule appointments, request prescription refills and receive educational materials, thereby enhancing patient engagement and streamlining administrative processes [9,10].
Asynchronous or Store-and-forward technology involves collecting medical data such as images, lab results and patient histories and transmitting them to healthcare providers for later review. This method enables specialists to assess and diagnose conditions without the need for real-time interaction, facilitating efficient consultations and care for patients in remote or underserved areas [8].
Efficiency
Telehealth has demonstrated equivalent if not superior, clinically effective outcomes compared to traditional in-person care across various medical disciplines [12,13]
Research across multiple disciplines reveals telehealth does not increase mortality rates and even reduces them in some cases. Early detection of disease exacerbation through remote patient monitoring (RPM) is often cited as a critical mechanism. For example, in cardiovascular care, telehealth has shown significant reductions in all-cause mortality among heart failure patients compared to traditional care models. Similarly, lower hospitalisation rates have been observed in these patients, and when hospitalisation does occur, telehealth patients experience shorter stays [12].
Telehealth has shown robust effectiveness in disciplines like psychology or psychiatry and endocrinology. Studies indicated that telehealth interventions are often as effective, if not more effective than traditional in-person care. Examples include a 20% lower risk of preterm births in obstetrics patients; good sensitivity, accuracy and specificity in skin cancer diagnosis utilising store-and-forward technology; reduced severity of mental health conditions like depression and comparable blood pressure control in nephrology patients [13].
It's important to note that evidence for efficiency is highly discipline-specific, and more research is needed across a wider range of medical specialities. While telehealth has demonstrated significant benefits in certain areas, the feasibility of remote healthcare delivery caries and many healthcare services will still require in-person interaction.
Regulations in Telehealth
Regulations governing telehealth vary significantly across different regions and can impact practitioners in various ways. The most stringent requirement universally is that healthcare providers must be licensed or registered with the relevant regulatory body to practice telemedicine. In the United States, practicing telemedicine without the proper license is a criminal offense, although such cases rarely result in prosecution due to practical enforcement challenges. In contrast, many other countries lack the authority to mandate that remote practitioners be licensed in the jurisdiction of their patients, creating a patchwork of regulatory environments. Besides licensing, other regulations related to telehealth, such as adherence to standards of care and privacy laws, are generally less binding and often enforced reactively rather than proactively. Violations of these standards are usually addressed on a case-by-case basis, often in response to specific complaints. While these requirements align closely with those for traditional healthcare services, the virtual nature of telehealth can sometimes obscure or complicate the detection of non-compliance, making enforcement a nuanced and evolving challenge [14].
Challenges
Technology access and literacy
· Ensuring equitable access to technology and internet connectivity is crucial for the effective implementation of telehealth services. Low socioeconomic status patients often lack the necessary resources, education, and understanding of technology, which significantly hinders their ability to benefit from telehealth.
· Inadequate telehealth access, compounded by limited resources, medication facility accessibility, and internet issues, disproportionately affects these patients, exacerbating health disparities [15,16].
Privacy, security & legal concerns
· Concerns about the safety, quality, confidentiality and data security in telehealth, with potential risks of compromised confidentiality
· Issues related to informed consent, treatment procedures, supervision of care providers, liability insurance and the increasing need for legislation to prevent fraud and misuse as telehealth usage grows [17].
Quality of care / Reduced Patient engagement and therapeutic relationships
· Virtual interactions may negatively impact patient engagement, empathy, emotional considerations and therapeutic relationships, reducing the stability of care
· Concerns about the lack of personal interaction and preference for in-person visits with familiar healthcare providers, especially during times of need [18].
Training and adaption
· Medical students and healthcare professionals will require specialised training to effectively utilise telehealth technologies. This includes how to operate telehealth platforms, conduct virtual consultations and manage remote monitoring systems.
· Telehealth training is not widely included in UK or US Medical degree courses. Medical curricula should incorporate telehealth training and technologies should be developed to train these skills effectively, ensuring future healthcare professionals are well-prepared for the evolving landscape of remote health [19].
The growing evidence of telehealth’s effectiveness, efficiency and potential to revolutionise healthcare delivery underscores the urgent need for investment and innovation in this field. By embracing and advancing telehealth technologies, we can improve access to care, enhance patient outcomes and bridge gaps in healthcare delivery. Investing in telehealth is an investment in the future of healthcare, promising a more connected, efficient and patient-centred system.
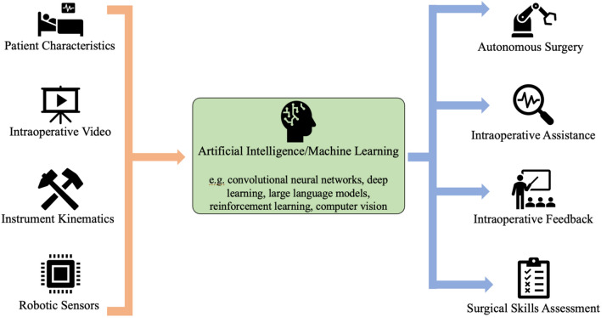
Role of AI
Artificial Intelligence (AI) plays a transformative role in enhancing telehealth by addressing both operational challenges and improving care delivery. AI's integration into telehealth can significantly streamline healthcare services through advanced data analysis and decision support systems. For instance, AI algorithms can efficiently match patients with clinicians based on specific skill sets, optimising the allocation of resources and improving the timeliness of care. Additionally, AI-driven tools enhance diagnostic accuracy and patient monitoring by analysing vast datasets to support personalised treatment plans and predict potential health issues before they escalate. Moreover, AI facilitates the development of innovative models of care, such as remote patient monitoring and virtual health assistants, which can provide continuous, personalised care and support patient engagement. As telehealth evolves, AI's ability to process and interpret complex health data will be crucial in addressing the growing demands for healthcare and overcoming the limitations of traditional delivery models. However, the deployment of AI in telehealth also necessitates careful consideration of ethical and equity issues to ensure that technological advancements enhance, rather than hinder, access to quality care [20].
Where to find out more
Romilly Life Sciences can offer several decades experience leading the validation, regulatory approval and implementation of telehealth solutions including country- and condition-specific patient journeys for rare diseases as well as national vaccination programmes.
To find out how you can reach patients faster, backed by compelling evidence, contact us.
References
[1] Federal Communications Commission (2014). Telehealth, Telemedicine and Telecare: What’s What? [online] Federal Communications Commission. Available at: https://www.fcc.gov/general/telehealth-telemedicine-and-telecare-whats-what.
[2] Khoshrounejad, F., Hamednia, M., Mehrjerd, A., Pichaghsaz, S., Jamalirad, H., Sargolzaei, M., Hoseini, B. and Aalaei, S. (2021). Telehealth-Based Services During the COVID-19 Pandemic: A Systematic Review of Features and Challenges. Frontiers in Public Health, 9. doi:https://doi.org/10.3389/fpubh.2021.711762.
[3] Bouabida, K., Lebouché, B. and Pomey, M.-P. (2022). Telehealth and COVID-19 Pandemic: An Overview of the Telehealth Use, Advantages, Challenges, and Opportunities during COVID-19 Pandemic. Healthcare, [online] 10(11), p.2293. doi:https://doi.org/10.3390/healthcare10112293.
[4] Corden, E., Rogers, A.K., Woo, W.A., Simmonds, R. and Mitchell, C.D. (2020). A targeted response to the COVID‐19 pandemic: analysing effectiveness of remote consultations for triage and management of routine dermatology referrals. Clinical and Experimental Dermatology, 45(8), pp.1047–1050. doi:https://doi.org/10.1111/ced.14289.
[5] Speyer, R., Denman, D., Wilkes-Gillan, S., Chen, Y., Bogaardt, H., Kim, J., Heckathorn, D. and Cordier, R. (2018). Effects of telehealth by allied health professionals and nurses in rural and remote areas: A systematic review and meta-analysis. Journal of Rehabilitation Medicine, [online] 50(3), pp.225–235. doi:https://doi.org/10.2340/16501977-2297.
[6] NIH (2020). Telehealth. [online] www.nibib.nih.gov. Available at: https://www.nibib.nih.gov/science-education/science-topics/telehealth.
[7] Taha, A.R., Shehadeh, M., Alshehhi, A., Altamimi, T., Housser, E., Simsekler, M.C.E., Alfalasi, B., Al Memari, S., Al Hosani, F., Al Zaabi, Y., Almazroui, S., Alhashemi, H. and Alhajri, N. (2022). The integration of mHealth technologies in telemedicine during the COVID-19 era: A cross-sectional study. PLOS ONE, 17(2), p.e0264436. doi:https://doi.org/10.1371/journal.pone.0264436.
[8] www.england.nhs.uk. (n.d.). NHS England» Purpose of the GP electronic health record. [online] Available at: https://www.england.nhs.uk/long-read/purpose-of-the-gp-electronic-health-record/#:~:text=The%20GP%20electronic%20health%20record%20forms%20the%20core%20of%20the.
[9] McAlearney, A.S., Sieck, C.J., Gregory, M.E., Di Tosto, G., MacEwan, S.R., DePuccio, M.J., Lee, J.A., Huerta, T.R. and Walker, D.M. (2021). Examining Patients’ Capacity to Use Patient Portals. Medical Care, 59(12), pp.1067–1074. doi:https://doi.org/10.1097/mlr.0000000000001639.
[10] Kaelber, D.C., Jha, A.K., Johnston, D., Middleton, B. and Bates, D.W. (2008). A Research Agenda for Personal Health Records (PHRs). Journal of the American Medical Informatics Association, 15(6), pp.729–736. doi:https://doi.org/10.1197/jamia.m2547.
[11] Di Xiao, Janardhan Vignarajan, Justin Boyle, Ming Zhang, Mohamed R Abdalla Estai, Marc Tennant, Mei-Ling Tay-Kearney, and Yogesan Kanagasingam. 2015. "Development and Practice of Store-and-Forward Telehealth Systems in Ophthalmology, Dental, and Emergency." Stud Health Technol Inform, 214: 167-173. PMID: 26210435.
[12] Snoswell, C.L., Stringer, H., Taylor, M.L., Caffery, L.J. and Smith, A.C. (2021). An overview of the effect of telehealth on mortality: A systematic review of meta-analyses. Journal of Telemedicine and Telecare, 29(9), p.1357633X2110237. doi:https://doi.org/10.1177/1357633x211023700.
[13] Snoswell, C.L., Chelberg, G., De Guzman, K.R., Haydon, H.H., Thomas, E.E., Caffery, L.J. and Smith, A.C. (2021). The clinical effectiveness of telehealth: A systematic review of meta-analyses from 2010 to 2019. Journal of Telemedicine and Telecare, [online] 0(0), p.1357633X2110229. doi:https://doi.org/10.1177/1357633x211022907.
[14] Europe Economics (2018) Regulatory approaches to telemedicine. [Report] General Medical Council. Available at: [https://www.gmc-uk.org/about/what-we-do-and-why/data-and-research/research-and-insight-archive/regulatory-approaches-to-telemedicine] (Accessed: 2nd August 2024).
[15] Breton, M., Sullivan, E.E., Deville-Stoetzel, N., McKinstry, D., DePuccio, M., Sriharan, A., Deslauriers, V., Dong, A. and McAlearney, A.S. (2021). Telehealth challenges during COVID-19 as reported by primary healthcare physicians in Quebec and Massachusetts. BMC Family Practice, [online] 22(1). doi:https://doi.org/10.1186/s12875-021-01543-4.
[16] Adler-Milstein, J., Kvedar, J. and Bates, D.W. (2014). Telehealth among US hospitals: several factors, including state reimbursement and licensure policies, influence adoption. Health affairs (Project Hope), [online] 33(2), pp.207–15. doi:https://doi.org/10.1377/hlthaff.2013.1054.
[17] Gajarawala, S. and Pelkowski, J. (2021). Telehealth benefits and barriers. The Journal for Nurse Practitioners, [online] 17(2), pp.218–221. doi:https://doi.org/10.1016/j.nurpra.2020.09.013.
[18] Portnoy, J., Waller, M. and Elliott, T. (2020). Telemedicine in the Era of COVID-19. The Journal of Allergy and Clinical Immunology: In Practice, 8(5). doi:https://doi.org/10.1016/j.jaip.2020.03.008.
[19] Jonas, C.E., Durning, S.J., Zebrowski, C. and Cimino, F. (2019). An Interdisciplinary, Multi-Institution Telehealth Course for Third-Year Medical Students. Academic Medicine, 94(6), pp.833–837. doi:https://doi.org/10.1097/acm.0000000000002701.
[20] Kuziemsky, C., Maeder, A.J., John, O., Gogia, S.B., Basu, A., Meher, S. and Ito, M. (2019). Role of Artificial Intelligence within the Telehealth Domain. Yearbook of Medical Informatics, [online] 28(01), pp.035–040. doi:https://doi.org/10.1055/s-0039-1677897.



Comments