5 Minute Healthtech Jargon Buster: Virtual and Augmented Reality in Healthcare
- Romilly Life Sciences

- Sep 30, 2024
- 6 min read
by Saoirse Wilson, Research and Communications Associate
Extended Reality (XR), consists of Augmented Reality (AR) and Virtual Reality (VR).
These are novel technologies which, powered by Artificial Intelligence (AI), are delivering a increasingly positive impact on healthcare systems, particularly in the area of education and training.
By understanding these technologies, their applications, and the regulatory landscape, you can make informed decisions and drive innovations that improve patient outcomes. They will overall increase efficiency within the healthcare sector and make the patient experience less intimidating.
Image Credit: Life Sciences Hub Wales
AR enhances the real-world environment by overlaying digital information, thus improving the user's perception and interaction with their surroundings. VR, in contrast, immerses the user in a fully digital environment, isolating them from the real world. Both technologies, powered by AI, bring transformative potential to various medical applications by leveraging data analytics and machine learning to enhance their functionality and outcomes.
Potential Benefits of VR and AR
The integration of AR and VR in healthcare promises potential significant advancements in surgical training, patient outcomes and operational efficiency. The four main areas in healthcare that are seeing benefit of these new technologies are training and education, mental health and wellbeing (of both patients and staff), rehabilitation and physiotherapy, and pain management.
AR can enhance surgical precision by providing real-time visualisation of critical anatomical information directly onto the surgical field. This application not only improves accuracy but also reduces the risk of surgical errors. VR also plays a crucial role in patient education by providing interactive and detailed visualisations of anatomical structures and medical conditions, facilitating better understanding and engagement for surgical procedures (Zhang, Lu and Khanduja, 2023).
VR can be highly effective in pain management, where immersive environments can distract patients from discomfort, thus reducing their reliance on pain medication (Gupta, Scott and Dukewich, 2017). In rehabilitation VR offers engaging and interactive exercises that aid stroke patients in regaining motor skills more effectively (Laver et al., 2018).
Furthermore, VR provides a safe and controlled environment for medical training, enabling students and professionals to practice procedures without real-world consequences. AI enhances these technologies by analysing patient data to tailor VR therapy programs and optimise AR surgical tools, leading to personalised patient care and advanced medical training. This is being developed in many areas, including in training apps for performing cataract surgery. This makes practicing surgeries more financially accessible to students, as the current method of interactive surgical training is the use of expensive cadavers.
AR and VR can benefit by creating immersive environments for therapy, simulating exposure scenarios for phobia treatment, and providing distraction during anxiety-inducing treatments, It enhances psychological presence in virtual environments, facilitating stronger connections between patients and therapists. Success stories like Cedars-Sinai Medical Centre’s VR program, which has treated over 3,000 patients highlight its effectiveness (Cedars-Sinai, 2020). If VR can deliver cost-effective, scalable, and accessible mental health care it will become a very valuable tool in this field.
Key Technologies and Approaches
AR’s application in surgical assistance involves projecting 3D images of a patient’s anatomy during operations, offering real-time guidance that enhances surgical accuracy. This technology minimises the need for large incisions, promoting quicker recovery times and better outcomes. In medical training, VR simulations recreate a variety of medical scenarios, from common procedures to complex cases, providing invaluable hands-on experience in a risk-free setting. For pain management, VR creates immersive experiences that divert attention from pain, significantly reducing the need for pain-relieving medicines.
In rehabilitation, VR provides interactive exercises designed to be engaging and therapeutic, aiding patients, particularly those recovering from strokes, in regaining motor skills. AI plays a critical role by analysing extensive patient data to develop personalised VR therapy programs and refine AR surgical tools, predicting complications and suggesting interventions, thus enhancing diagnostic accuracy and patient care.
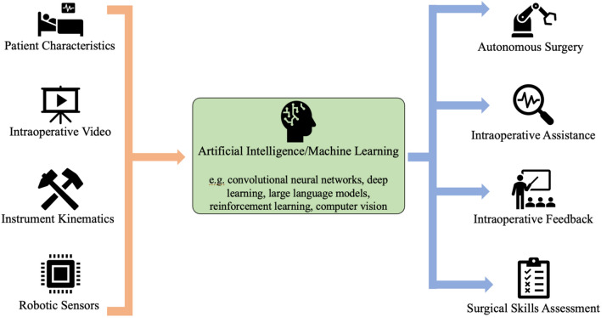
The Role of AI
Artificial intelligence (AI) significantly enhances AR and VR applications in healthcare through powerful data analytics and machine learning capabilities. AI algorithms analyse patient data to create personalized VR therapy programs and improve AR surgical tools by predicting complications and suggesting interventions. This leads to better diagnostic accuracy, personalized patient care, advanced medical training, and increased patient engagement. AI-powered image analysis and predictive analytics enable precise, real-time guidance in AR surgeries and customized VR rehabilitation programs. In medical training, AI-driven VR creates adaptive, interactive simulations, while AI also offers interactive education tools and virtual consultations. Additionally, the use of AI can optimise healthcare operations by managing data and ensuring regulatory compliance. By integrating AI, AR and VR can revolutionize healthcare, making treatments more effective and personalized, while overcoming many implementation challenges.
Challenges for the Technology
Despite the potential benefits, implementing AR and VR in healthcare presents several challenges. The high cost of these technologies is a significant barrier to widespread adoption. The initial investment required for hardware, software, and training can be prohibitive for many healthcare institutions (Bergin and Craven, 2023)
Additionally, the efficacy and safety of AR and VR applications need robust clinical validation through extensive trials and peer-reviewed studies. Without substantial evidence, gaining acceptance from medical professionals and regulatory bodies is challenging (Tang et al., 2019).
Cybersecurity risks are another major concern. The sensitive nature of data collected by AR and VR technologies makes them prime targets for cyber-attacks. Ensuring the security of this data through robust management systems is critical to comply with stringent regulations.
There are also privacy and ethical concerns related to patient consent and data usage. Ensuring that patients are fully informed about how their data will be used and obtaining explicit consent is essential. Ethical considerations around the use of immersive technologies in sensitive medical contexts also need to be addressed.
Implementation Solutions
Addressing these challenges requires a multifaceted approach. Increased investment in research is crucial for conducting robust clinical trials that provide solid evidence for the efficacy and safety of AR and VR technologies. This evidence is necessary to gain acceptance from the medical community and regulatory bodies (Mitchell and Ivimey-Cook, 2023).
Developing scalable and cost-effective AR and VR solutions can help make these technologies more accessible, encouraging broader adoption. Collaborative efforts between technology developers and healthcare providers can distribute costs and resources more efficiently (Bruno et al., 2022).
Enhanced cybersecurity measures are essential to protect sensitive patient data. Implementing advanced encryption techniques, regular security audits, and continuous monitoring can safeguard against cyber threats. Additionally, clear ethical guidelines and robust patient consent protocols must be established to address privacy concerns. This includes ensuring that patients are fully aware of how their data will be used and obtaining their explicit consent before collecting any information.T
Broader Applications
Beyond their specific medical applications, AR and VR technologies have broader implications for healthcare challenges. For instance, they can facilitate remote consultations by providing interactive patient education tools that help patients better understand their conditions and treatment options. In mental health, VR can create therapeutic environments that aid in managing stress, anxiety, and other mental health issues. By integrating AI, AR, and VR, we can revolutionize healthcare, making treatments more effective and personalized. These technologies hold the potential to significantly improve patient outcomes, streamline healthcare operations, and enhance the overall patient experience.
In conclusion, while AR and VR technologies face several challenges, their potential to transform healthcare is immense. By addressing these challenges through targeted research, cost-effective solutions, enhanced security, and clear ethical guidelines, we can unlock the full potential of these technologies to improve patient care and healthcare delivery.
Where to find out more
Romilly Life Sciences can offer several decades experience leading the validation, regulatory approval and implementation of healthcare solutions using cutting edge technologies such as VR, AR and XR as well as AI to solve real world, large scale clinical problems.
To find out how you can reach patients faster, backed by compelling evidence, contact us.
References
Bergin, A. and Craven, M.P. (2023). Virtual, augmented, mixed, and extended reality interventions in healthcare: a systematic review of health economic evaluations and cost-effectiveness. BMC Digital Health, 1(1). doi:https://doi.org/10.1186/s44247-023-00054-9.
Bruno, R.R., Wolff, G., Wernly, B., Masyuk, M., Piayda, K., Leaver, S., Erkens, R., Oehler, D., Afzal, S., Heidari, H., Kelm, M. and Jung, C. (2022). Virtual and augmented reality in critical care medicine: the patient’s, clinician’s, and researcher’s perspective. Critical Care, [online] 26(1). doi:https://doi.org/10.1186/s13054-022-04202-x.
Cedars-Sinai. (2020). VR and the Future of Healthcare. [online] Available at: https://www.cedars-sinai.org/blog/virtual-reality-future-healthcare.html.
Gupta, A., Scott, K. and Dukewich, M. (2017). Innovative Technology Using Virtual Reality in the Treatment of Pain: Does It Reduce Pain via Distraction, or Is There More to It? Pain Medicine, 19(1), pp.151–159. doi:https://doi.org/10.1093/pm/pnx109.
Laver, K.E., Lange, B., George, S., Deutsch, J.E., Saposnik, G. and Crotty, M. (2018). Virtual Reality for Stroke Rehabilitation. Stroke, 49(4). doi:https://doi.org/10.1161/strokeaha.117.020275.
Mitchell, A.A. and Ivimey-Cook, E.R. (2023). Technology-enhanced simulation for healthcare professionals: A meta-analysis. Frontiers in medicine, 10. doi:https://doi.org/10.3389/fmed.2023.1149048.
Tang, K.S., Cheng, D.L., Mi, E. and Greenberg, P.B. (2019). Augmented reality in medical education: a systematic review. Canadian Medical Education Journal, 11(1). doi:https://doi.org/10.36834/cmej.61705.
Zhang, J., Lu, V. and Khanduja, V. (2023). The impact of extended reality on surgery: a scoping review. International Orthopaedics. doi:https://doi.org/10.1007/s00264-022-05663-z.



Comments