5 Minute Healthtech Jargon Buster: Biomarkers
- Romilly Life Sciences

- Nov 17, 2023
- 1 min read
Updated: Nov 18, 2023
A biomarker (short for “biological marker”) is an objective measure that captures what is happening in a cell or an organism at a given moment. Biomarkers can serve as early warning systems for your health [1].

Image Credit: Research Advocacy Organization [2]
Formal definition of a biomarker
In 1998, the National Institutes of Health Biomarkers Definitions Working Group defined a biomarker as “a characteristic that is objectively measured and evaluated as an indicator of normal biological processes, pathogenic processes, or pharmacologic responses to a therapeutic intervention"[3]. A joint venture on chemical safety, the International Programme on Chemical Safety, led by the World Health Organization (WHO) and in coordination with the United Nations and the International Labor Organization, has defined a biomarker as “any substance, structure, or process that can be measured in the body or its products and influence or predict the incidence of outcome or disease” [4]. An even broader definition considers not just incidence and outcome of disease, but also the effects of treatments, interventions, and even unintended environmental exposure, such as to chemicals or nutrients [5].
Examples of biomarkers
Blood pressure, body temperature and body mass index are all biomarkers. However, biomarkers are not restricted to things that could be measured at a routine doctor's appointment. For example, we can also consider the level of gene expression within cells, or proteins within bone, as biomarkers [6].
Biomarkers, diagnostics, and artificial intelligence
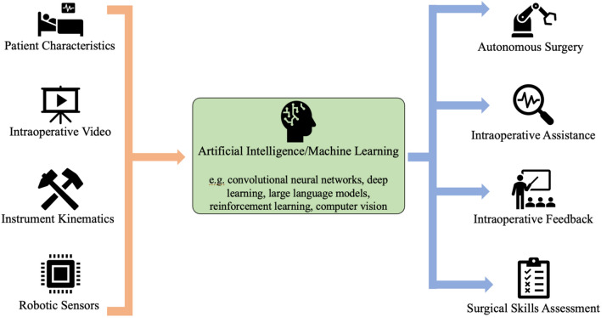
A diagnostic biomarker detects or confirms the presence of a disease or condition of interest or identifies an individual with a subtype of the disease [7]. Biomarkers are tied directly to the presence of a substance or process indicative of a disease. Artificial intelligence approaches such as machine learning have the potential to directly indicate treatment response/ disease progression by combining data from genomics, proteomics, metabolomics, and other omics, but also from oncology clinics, imaging, epidemiology and more into a single marker for complex and prevalent conditions including cancer [8], cardiovascular disease [9] and Alzheimer’s disease [10]. Further examples exist in the case of pathology [11] which traditionally entails laborious expert interpretation of stained tissue samples, while artificial intelligence has been applied to DNA samples to calculate the stiffness of tissue, known to alter the efficacy of breast cancer drugs, so that the clinical team can adapt treatments to be more effective in individual patients [12].
Biomarker evidence requirements
With any new measurement, a challenge is how to establish accuracy and clinical usefulness that goes beyond the existing state of the art, also known as the “gold standard “. The key activities to demonstrate the performance of any biomarker are Validation, Qualification and Utilisation [13]. Analytical validation involves demonstration of the accuracy, precision, and feasibility of biomarker measurement. If a biomarker cannot be reliably measured, it will have little or no use as an indicator for a biological process or clinical outcome. Key criteria include sensitivity (whether the biomarker can detect the underlying biological process of interest) and specificity (whether the biomarker gives a negative result when the process is not present). Qualification involves demonstrating that a biomarker is associated with a clinical endpoint. Also known as clinical validation, a clinically valid test will often correlate with improvement in patient care [14]. Utilisation (or clinical utility) involves the assessment of biomarker performance in the specific context (e.g. hospital environment) of its proposed clinical use. This supports use of a biomarker as providing benefits to the patient that outweigh any potential drawback (e.g. the need for an invasive procedure such as a biopsy to sample the biomarker).
Regulation of biomarkers
Ultimately the need for regulation depends on the intended use of the biomarker. When a biomarker is qualified, it means that it has undergone a formal regulatory process to ensure that we can rely on it to have a specific interpretation and application in medical product development and regulatory review, within the stated context of use. It is important to note that at this point only a biomarker is qualified, and not the biomarker measurement method.
Often biomarker measurement methods that rely on a biological test sample (for example blood or tissue) are considered as In Vitro Diagnostics and treated in a similar way as medical devices, such as medical image-based diagnostic biomarkers which have to be assessed and approved by a national authority before they can be put onto the market. Depending on how samples are acquired and analysed, the use of laboratory facilities as well as biological products may also bring in other regulatory requirements such as Clinical Laboratory Improvement Amendments (CLIA) or Good Clinical Laboratory Practice (GCLP). While biomarkers that are used in research settings may not be obliged to meet these standards, programs exist to help standardise approaches and to promote their use. For example, the FDA Biomarker Qualification Program [15] is based on the understanding that qualified biomarkers have the potential to provide valuable information that may reduce uncertainty in regulatory decisions during drug development. The Quantitative Imaging Biomarkers Alliance (QIBA) initiative from the Radiological Society of North America (RSNA) has proposed an imaging biomarkers qualification profile that is being adopted among different types of imaging measurements procedures [16]. In the UK, the National Physics Laboratory has supported the qualification of a range of biomarkers.
Where to find out more
Romilly Life Sciences can offer several decades experience leading the validation, qualification and utilization of a range of novel biomarkers including brain function activity from MRI, breast cancer detection using microwave radar and machine learning to generate new imaging-based cancer endpoints for clinical trials.
To find out how we can help you commercially develop the next gold standard, contact us.
References
[2] https://researchadvocacy.org/sites/default/files/resources/BiomarkerValidationFinal-vDownload.pdf


Comments